Abstract
Introduction: Lymphoblastic lymphoma (LBL) is a rare and aggressive neoplasm which is more common in children and young adults. The adoption of pediatric inspired regimens for acute lymphoblastic leukemia (ALL) increased response rates and improved overall survival (OS). Due to the rarity of this disease studies addressing specific outcomes of LBL, especially from Latin America, are lacking.
Objectives: To report outcomes of adult newly diagnosed with LBL in our center, aiming to examine baseline factors associated with worse survival.
Methods: Retrospective cohort study of patients diagnosed with LBL between 2002 and 2018 and treated with adapted-BFM (aBFM) regimen at Instituto do Cancer do Estado de São Paulo (ICESP). Patients with acute leukemia were excluded from this analysis. The aBFM protocol was based on the BFM-86 protocol and previously reported by our group (Pinheiro et al, 2006).
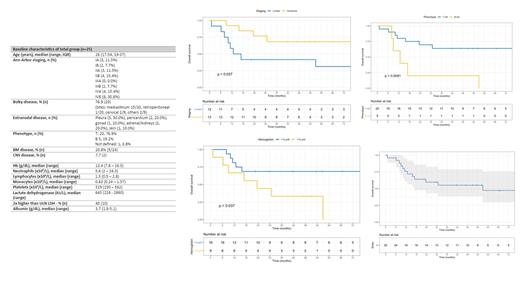
Results: Over this period, 26 patients received aBFM protocol in our institution. Twenty patients had T-LBL (77%) and mostly male (n=18). Median age was 26 years (17-54). Fifty-four percent (n=9) had an advanced stage (III-IV) and 77% (n=20) had bulky disease at diagnosis, predominantly mediastinal (n=15). Bone marrow involvement occurred in 21% of cases (5/24) and CNS disease was found in 2 cases. Complete remission (CR) rate was 68% (17/25). Four out of 5 B-LBL cases did not achieve CR, showcasing the influence of immunophenotype on CR (p=0.04). Two patients died before response assessment. Nine patients underwent consolidation radiotherapy (RT), defined at the discretion of the physician. The remaining 2 cases received cranial RT for CNS involvement. At 5 years, overall survival (OS) was 47,3% (CI 95%, 29,5 - 75,6) and event-free survival (EFS) was 51,1% (CI 95%, 34,6 - 75,5). Univariate analysis showed that phenotype (B-cell, HR=4.3) and the hemoglobin level at the diagnosis (continuous, HR=0.78) were significantly associated with OS (Figure). Cumulative incidence of relapse was 36%, whereas non-relapse mortality was 12% in this cohort.
Discussion: Current treatment of LBL is based on pediatric ALL protocols including CNS prophylaxis. Previous studies of LBL patients using pediatric inspired regimens had 3y OS of 69%, which is higher than that found in our study. Markedly, outcomes of patients with B-LBL were poor and notably, no genetic evaluation aiming to screen for BCR-ABL or Ph-like signature was performed in such cases. These genetic alterations are more common in Latin America and must be screened as they strongly impact on the management.
Conclusions: Few studies encompassing adult LBL patients are available. To our knowledge, this is the first one from Brazil. Although this study carries several limitations, we can conclude that the use of aBFM is feasible and achieves acceptable response rates in the T-cell subset. By contrast, B-LBL cases fared poorly and further studies are needed to implement a better genetic characterization and newer treatment strategies.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal